Neck Pain
According to the Global Burden of Disease 2010 study, neck pain is the fourth leading cause of years lost to disability, ranking behind back pain, depression, and arthralgias (2013). It is believed that half of all individuals will experience a neck pain episode over the course of their lifetime (Fejer et al. 2006). The prevalance of neck pain is higher in females and peaks in middle age. Neck pain is associated with headaches, back pain, joint pain, and depression.
Who Gets Neck Pain?
Variables associated with neck pain include genetics, depression, anxiety, poor coping skills, sleep disorders, smoking, and sedentary lifestyle with very little physical activity. Other risk factors for neck pain include trauma (brain and whiplash injuries), and certain sports injuries. There are certain occupations such as office workers, manual laborers, and health care workers to have a higher incidence of neck pain, the major factors are low job satisfaction and percieved poor wokplace environment.
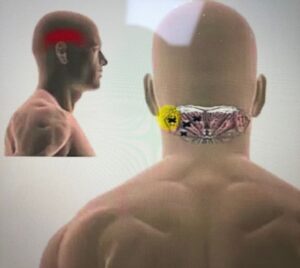
Neck Pain Mechanisms
Neck pain categorised by mechanisms as mechanical (pain originating in the spine or its supporting structures, such as ligaments and muscles). Common strutures for the cause of mechanical pain are facet joints (arthritis), discs, and pain from muscles and fascia. Nerve pain refers to the peripheral nervous system, which involves mechanical or chemical irritation of nerve roots. The most common examples of nerve pain are symptoms from a herniated disc or osteophyte (pointed outgrowth of bone) and spinal stenosis (narrowing of space within your spine). Differentiating nerve pain from mechanical pain is an important part of the clinical assessment and will influence your management.
Natural course of Neck Pain
Acute neck pain that has lasted for <6 weeks will resolve within 2 months but half of the patients can continue to have frequent recurrences 1 year after occurence. Patients with cervical radiculopathy (pain referred into shoulder, arm, and hands with numbness and weakness and a decrease in function) have greater likelihood of ongoing pain.
Radiographs and MRI Scans

Patients with suspected structural abnormalities (e.g. scoliosis, fractures) plain X-rays are generally sufficient. MRI is sensitive for detecting soft-tissue (e.g. disc) abnormalities but MRI scans can produce results of high rate of abnormalities in individuals who do not have any symptoms or pain. Therefore, MRI is useful to rule out serious or progressive nerve deficits and when refering patients for surgery. That is why you may wonder and be furious with your GP or the specialist as to why they have not referred you for an MRI scan, they will not do so if they feel it is not that serious and most likely be successfully managed conservatively.
Treatment
Clinical trials have found that exercise may be beneficial, and for acute pain, muscle relaxants are effective. Spinal manipulations and massage therapy are often seen on social media platofrms such as Instagram to treat neck pain. These interventions are designed to maximise movement, reduce muscle tightness, improve joint mobility. The evidence suggest that they are superior to no treatment in the short-term but no over the long-term. To achieve better results over the long term, other factors such as stress, sedentary lifestyle, poor sleep, anxiety, smoking, and depression will have to be addressed and managed apppropriatley to reduce your neck pain. Thank you for reading and I hope this information helps you gain a better understanding.
References
US Burden of Disease Collaborators. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591-608.
Cohen, S. P. (2015). Epidemiology, Diagnosis, and Treatment of Neck Pain. Mayo Clinic Proceedings, 90(2), 284–299.