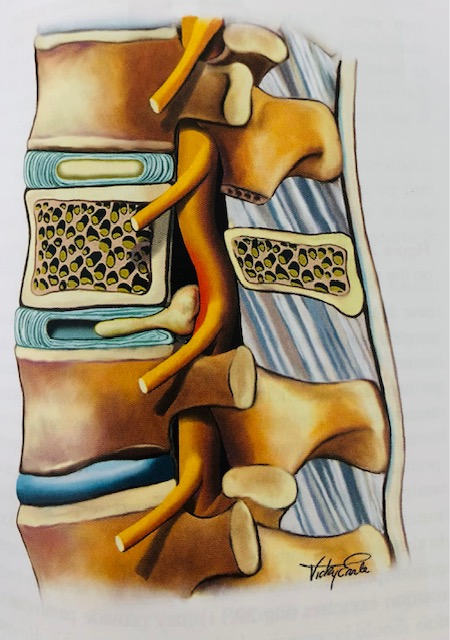
This picture shows a disc herniation irritating the nerve in the low back causing leg symptoms.
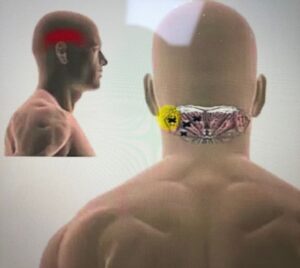
What is a Disc Herniation? Or what some call it, ‘slipped disc’
Each vertebral body consists of a disc which is made up of material called annulus fibrosus and within the annulus fibrosus is disc material/fluid called nucleus pulposus. The discs are firmly placed up above and below by vertebral endplates making it impossible for discs to ‘slip.’ The role of the discs is to promote movement, shock absorption, and the transfer of load. A disc herniation is thus defined by Fardon et al 2014, as the ‘localised or focal displacement of disc material beyond the normal margin of the disc space’, which can be classified as protrusion, extrusion, or sequestration. A bulging disc is often seen on an MRI image but that is not considered as a disc herniation.
Can a Disc Herniation heal?
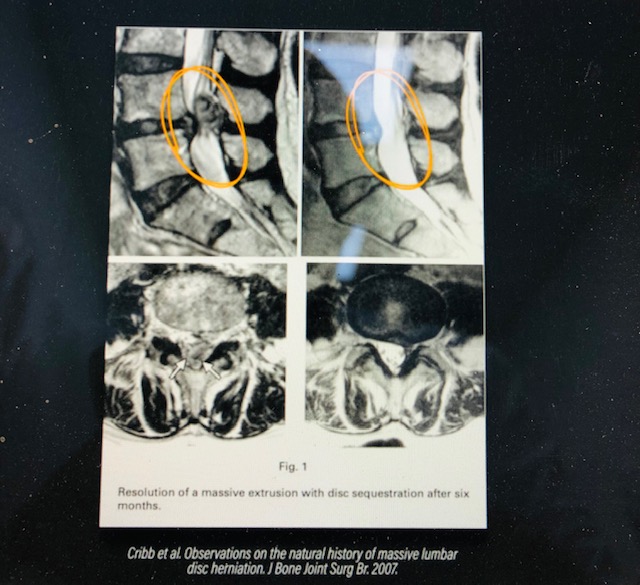
The answer is yes, the disc herniation can heal on its own without any intervention. This has been supported by different research studies by Chiu et al 2015, Zhong et al in 2017, and Wang et al in 2020. There is an image (below) which demonstrates this example in which a disc herniation significantly regressed/resorbed over time.
What will the MRI Image tell us?
MRI image will sometimes not tell us the full story. Here are some of the things you should know:
- Abnormalities are common to find in the spine of people who are asymptomatic. A review carried out by Brinkikji et al 2015 found that 29% of asymptomatic 20 year olds have a disc protrusion/disc bulges and this number increases with age.
- The sizer of the disc herniation does not matter or correlate with symptoms, even large disc herniations can heal. This was found by Karpinnen et al 2001, Benson et al 2010, and Gupta et al 2020.
- You can become asymptomatic despite the disc herniation still being present on the MRI (Benson et al. 2010).
- More compression of the nerve in the spine does not mean more symptoms, pain is complex and multifactorial. Rijn et al 2006 found nerve compression in people but without symptoms.
Is Surgery required for your low back pain?
The short answer is, most people will not require surgery, and this is supported by research.
People who have had surgery, the long-term outcomes are no better than people who did not have surgery (Fernandez et al. 2016). There is evidence that surgery may be better in the short term for pain and function but long-term the results are no better than non-surgical management (Paul et al.2007; Overdevest et al. 2014).
Surgery may be recommended when severe and progressive nerve symptoms are present such progressive pain, numbness and leg weakness and reduced function is present.
An MRI scan is discouraged for at least 6 weeks unless symptoms are not improving and after attempting non-surgical management.
What can you do to manage your symptoms?
- Take notice of the posture and positions that is aggravating your pain such as, sitting for long periods may increase your pain, so you may not want to sit down for too long. Take notice of your sitting position when driving, watching TV, using your mobile phone, and see if you can modify those positions to reduce your pain and symptoms.
- You may want to exercise, any exercise is good, and there is no ONE type of exercises that are found to be more beneficial than others, so general movement and mobility is good and pick some exercises which you prefer.
- Living a healthier lifestyle is also going to help with healing. You can begin to develop healthier habits such as no smoking, eating well, sleeping well, exercising regularly, staying hydrated.
Summary
Disc herniations can heal, sometimes it can take up to 6 months to heal, MRI scan doesn’t always tell the full story, wait at least 6 weeks before requesting a MRI scan, and surgery is most of the time not required. Try and find comfortable exercises to do, pick any of your choice, walking is good and helpful in reducing your time sitting for prolonged periods.